- Eligibility
- Registering
- Practical information
- Procedure
- Use of brain tissue, type of research & results dissemination
- Privacy
1. Who may donate?
Every participant in the Luxembourg Parkinson’s Study who resides in Luxembourg may donate their brain. Being able to correlate post-mortem brain analysis with molecular and clinical study results is an invaluable resource for research. Therefore, the brain collection is dedicated to collecting the brains of donors involved in the study.
People with and without Parkinson’s disease are invited to participate in this research programme. People without Parkinson’s disease are as important as patients as they will be ‘control persons’ and serve as a reference for comparison with patients. Both patients and healthy volunteers can then register as brain donors.
Legally, any competent person over 18 years of age may donate his/her brain after giving consent during his lifetime. Consent can be given by a legal representative for people who are not able to give their consent themselves.
2. Do I need to have a brain disorder to become a donor?
No. Anyone can become a donor - irrespective of whether you have a brain disease or not. Healthy brain tissue - known as “control tissue” - is just as important to research as tissue donated by patients. During scientific studies, researchers often need to compare tissue samples from patients with neurological diseases to control tissue.
3. Can I become a donor if I live in the Greater Region?
No. You have to live in Luxembourg to become a donor. As post-mortem tissue must be collected and stored as soon as possible after death to be useful to researchers, distance is an obstacle. If you live in a neighbouring country and wish to become a donor, you could contact the nearest brain bank.
4. What might prevent the donation?
While we do everything we can to ensure that a donation takes place, it may not always be possible. Ideally the brain tissue must be obtained within 24 hours after death but can be collected up to 48 hours after death. If there is a delay (lack of available resources over weekends and holiday periods), it may not be possible to take samples of good enough quality for research. In this case, we will not go ahead with the tissue retrieval. We do our best to avoid delays by closely liaising with families and professionals.
5. Does donating brain tissue for research purposes interfere with religious beliefs?
None of the major religions has an absolute veto of autopsies. Christian denominations raise no general objections to autopsies. Judaism and Islam accept the autopsy provided that its usefulness and necessity are demonstrated. Buddhism and Hinduism see this act as an individual decision.
6. Is it possible to be registered as an organ donor as well?
Yes. Organ donation and brain donation are separate matters, as – in contrast to kidneys or other organs - brains will not be transplanted. Of course, you can register for both. However, as most deceased organ donors are brain-dead (i.e. they have suffered complete and irreversible loss of all brain function), it will often prevent brain donation.
1. How do I donate my brain?
If you wish to be a donor, we invite you to register with the NCER-PD brain donor programme and to state your wishes ahead of time in writing. The procedure is free and straightforward.
You and a person of trust chosen by you (a relative or a legal representative) will need to make an appointment at the clinic and complete a consent form. This form will allow NCER-PD to collect the brain tissue after death.
If you wish to book an appointment or if you need any specific advice and further information, please do not hesitate to contact our team (+352 4411 4848 or parkinson@chl.lu). We will be happy to answer your questions and guide you through the process.
2. What if you decide to withdraw after giving consent?
You are free to withdraw your consent at any time. Your decision will be fully respected, no questions will be asked and there will be no impact on your participation in the Luxembourg Parkinson Study. If you have any questions once you have registered, please contact the NCER-PD team (+352 4411 4848 or parkinson@chl.lu).
3. Does my doctor need to know that I intend to donate my brain upon my death?
We recommend that you inform your family doctor. In case of death outside the hospital, he will be asked to complete the death certificate. It is therefore important that he is aware of your choice so that procedures can be quickly carried out.
4. Do I have to tell my relatives?
It is not mandatory, but we recommend that you share your decision with your family members. Your relatives might need time to discuss this very important issue and talking about brain donation with your next of kin will also help ensure your wishes are considered.
It is also important to make the necessary arrangements for the brain donation well in advance and at least one family member will need to be involved in these preparations. Everyone concerned should know that in the event of death someone needs to immediately call the NCER-PD team.
5. Who can legally grant permission for an autopsy to be performed?
After death, if the deceased did not state his/her wishes ahead of time in writing, the legal next of kin must authorise the autopsy before it can be performed. The persons that may provide such consent are for example (in order of priority) the spouse, adult sons and daughters, parents, brothers and sisters or a guardian. If there are several family members with the same priority level, they have equal authority and must all agree.
Are there costs for the donor or family?
No. Neither you nor your relatives will incur any costs. The brain bank will cover all costs involved with transportation of the body for the procedure and associated with the brain donation. Funeral expenses however, remain the responsibility of the family the same as they would if donation was not made.
2. Are there incentives for brain donation?
Donation is voluntary and has no financial benefits. The decision to donate can be difficult and each donor has his or her personal motivations but most of them share a common satisfaction in knowing that they are helpful after death and are contributing to research for future generations.
3. Will brain donation interfere with funeral arrangements?
No. The donation procedure does not interfere with the normal course of events associated with a funeral. Since the tissues are removed as soon as possible after death, it is unlikely that donation will delay arrangements for the funeral. Usually the procedure takes between three and four hours and the donor will be released back into the care of the funeral director on the same day or in some cases the following day. NCER-PD will work closely with families and funeral homes to ensure that donation does not interfere with or delay funeral arrangement.
4. What will the person look like after the brain tissue has been removed? Can he/she have an open casket viewing?
The procedure used for removing the tissues does not cause any visible disfigurement and a normal viewing of the deceased with an open casket can be planned. All the procedures are performed with the utmost respect for the individual who donated the tissues.
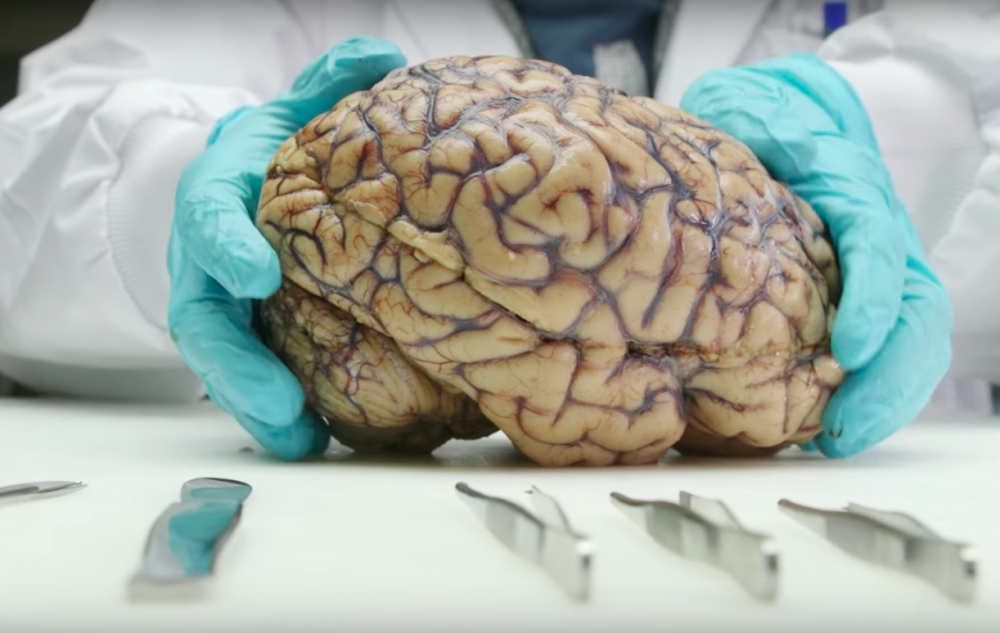
After the confirmed death of a registered donor, the brain tissues are removed during an autopsy. The post-mortem examination is carried out by a pathologist, ideally within 24, but up to 48 hours after death. Usually, a brain autopsy takes 3 to 4 hours.
In the framework of the Luxembourg Parkinson’s Study, the entire brain is collected, including the brain stem (tissue from the top of the spine).
For patients, the brain tissue will allow a definitive diagnosis of the underlying cause of parkinsonism. A definitive diagnosis is needed before the tissue is made available for research. After that, the brain tissues will be prepared and be stored safely and securely for their ethical use in scientific research.
2. What happens after the autopsy?
The brain is prepared for research according to standardised protocols. Parts of the brain are frozen and stored so that it remains optimally preserved for use in research. It will be processed into individual tissue samples to ensure that each donation provides material for as many research projects as possible. Other parts will be fixed in formalin for 2-3 weeks to preserve the tissue. Afterwards tissue samples will be taken for paraffin embedding, i.e. it is placed in a wax for conservation purposes. The whole process can take some months to achieve. All these procedures are performed with the utmost respect for the individual who donated the tissues.
1. How will the tissue be used?
(The brain tissue will first allow a definitive diagnosis of the underlying cause of parkinsonism. Afterwards, the brain tissue will be made available for research. The tissues will be stored safely and securely for their ethical use in scientific research.)
In accordance with NCER-PD framework, the donated tissue will be used for high-quality research in both Luxembourg and abroad, in the public or private sector. The research projects supplied with the tissues aim to improve understanding, diagnosis and treatment of neurodegenerative disorders, especially Parkinson’s disease.
Researchers who wish to have access to brain samples have to contact the NCER-PD steering committee and submit an application. To receive the approval of the team, a research project has to be both ethically appropriate and scientifically sound. This means applicants must show that they have the expertise to perform their proposed research, that the proposed research has ethical clearance, and that they have sufficient funds to see the research through to completion. This way, the samples are only shared with proven research groups and everyone receiving tissue from the brain collection agrees to the same terms and conditions.
2. How long will the tissue be stored and how will it be disposed of?
No specific time limit is set for the storage of samples. The preservation techniques ensure that tissues will remain usable in research for many years. The samples obtained from one brain can supply research projects for ten years or more. Samples are regularly checked and are only disposed of if their quality is insufficient for research use. The disposal of the tissues is done in an ethical and respectful manner.
3. Can I find out how my relative’s brain was used and what research it contributed to?
NCER-PD will ensure that donated tissues are used for high-quality research but cannot give out information about the exact type of research your relative’s brain will contribute to. Indeed, the majority of the studies that will use samples from the brain bank are not known yet and for this reason it is not possible to inform the donors or their families in advance of the exact nature of the research, where or when it will be carried out or by whom. All the tissue used by researchers are contributing to understand further the brain and neurological diseases such as Parkinson’s disease.
4. Will the tissue be used in any genetic studies?
Genetic studies may be performed in some instances. Such studies will require prior consent by the participant during lifetime, and the use of samples and data will be mandated to take place in accordance with the informed consents given by the participants. Genetic material of participants who have consented, both patients and controls, can be subjected to Next Generation Sequencing (NGS) technologies. Resulting data will be used for clinical stratification of the different forms of parkinsonism.
5. Will the family be informed of the results of the genetic research?
The brain bank does not report individual research results or findings routinely. Samples are donated for scientific inquiry and not for clinical decision making. However, researchers who come across findings in a sample, that have a robust, widely accepted, scientifically proven impact on prognosis or risk, can inform the NCER-PD study team. If the relatives of the participant concerned by this finding stated that they wish to be informed in such a case, and if a panel of experts decides that this information is relevant for the family, they will be contacted through a physician.